Nipple pain if your baby is breastfeeding:
It can take some time to feel confident with positioning and attaching your baby at the breast, particularly if they were born a bit early. Don’t forget that you are both just learning! There is lots of support available to help get things off to a good start. Your nipple should be right at the back of your babies mouth, if it is pressed against the roof of your baby’s mouth during a feed this can cause damage and pain. Ask a member of nursing staff or infant feeding team to observe a feed and offer information and support to make sure your baby is well attached. If you experience pain or discomfort during a feed, use a finger to very gently ease your baby from the breast and reposition. Ask for information on other positions to try until you find what works well for you.
Tongue tie
Tongue-tie is where the piece of skin connecting the tongue to the bottom of the mouth is shorter or tighter than usual. This can sometimes cause nipple pain and challenges with breastfeeding. Not all babies who have a tongue tie have challenges with feeding. It is important that diagnosis includes a skilled assessment of feeding and tongue function. If you are worried that your baby has a tongue tie speak to your nurse who can refer you to the infant feeding team and then ENT if needed.
Nipple pain if expressing:
Using the breast pump should not cause discomfort or damage to your nipples. If you do find this uncomfortable, check that you have the correct funnel size for you. Nipples come in all shapes and sizes, and so we have lots of options for funnel size too. There should be enough space for your nipple to move freely, but not so much space that your areola (the area surrounding your nipple) is also within the funnel. If in doubt ask a member of staff to help you assess this. Check also that the vacuum is not turned up too high – turn the dial until you feel slight discomfort then go back a level or two until you feel comfortable. Expressing should be sustainable and pain-free!
This page on the Medela website shows you how to check the shield size is correct
Self care for nipple pain:
Wear a supportive cotton bra and change this regularly, if using breast pads try to avoid those with plastic-backing and change when they become damp. Express breast milk onto your nipples to help with healing and expose to the air when possible. Continue to feed/express as normal.
Breast pain
It is normal for your breasts to feel full and uncomfortable in the early days after your baby is born, and there are some simple steps you can take to ease this discomfort. Wearing a well-fitting, supportive non-wired bra is important. You may find that your usual bra size will change so if you can, get measured or measure yourself to determine the best size for you.
Engorgement
If your breasts are engorged, they may feel hot, lumpy and painful. This can happen while you are establishing your supply of breast milk, or later down the line if you have a bigger gap than usual between feeds or expressions. Again, a well-fitting bra will help to support your breasts and relieve some discomfort. You may find that a hot or cold pack is beneficial too. If your baby is feeding from the breast, they may find it more difficult to attach to a very full breast; hand expressing some milk beforehand will make things easier. If expressing, try not to leave big gaps between sessions.
Mastitis
Mastitis means ‘inflammation of the breast’ and covers a wide range of symptoms, such as heat, pain, redness, a lump in the breast or nipple discharge. This leaflet from the Breastfeeding Network has lots of information on the causes and treatment if you are experiencing Mastitis. If you feel flu-like or unwell it is important to let a member of staff know, so that you can be assessed for infection and supported to manage the symptoms.
Breastfeeding Network Mastitis leaflet
Dwindling supply
You may find that while your baby is in the neonatal unit your supply may fluctuate, particularly if your baby is not quite ready to feed from the breast. You may find it helpful to use the ‘Expressing Log’ to keep track of how much milk you collect each time. If you notice that this has reduced there are lots of things we can do to help get you back on track. There is a very useful Expressing Assessment Chart in your ‘Feeding Journey’ booklet which either you or a member of staff can use to consider if any tweaks need to be made to your expressing regime. Checking the size of your pump funnel can help too, as the size you need may change over time. Make sure you have lots of skin to skin cuddles with your baby and allow them to nuzzle and lick at the breast – this will help boost the hormones needed to produce milk and is a lovely chance to help you relax and let your baby practice feeding. Speak to a member of staff at the earliest opportunity so we can support you to get your milk supply back on track.
Expressing and breastfeeding assessment tools
There are lots of resources available to help with your breastfeeding and expressing goals. Every baby in the neonatal unit will have a booklet called ‘My Feeding Journey’ which has lots of useful information and tools for you and the neonatal staff to use.


This includes a handy checklist for assessing when expressing is going well, and things to try if you have concerns.
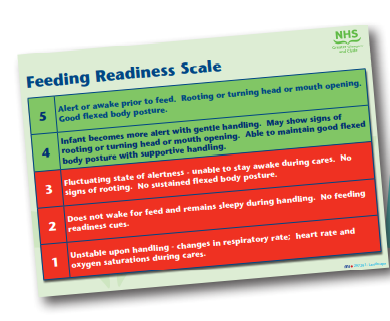
There is also an assessment chart for when your baby is ready to start feeding from your breast which will help you to see your baby’s progress and support you with moving towards responsive breastfeeding.

There are pages for notes which the nursing staff and infant feeding team will use to record any support given. You can also use them to write down your thoughts about expressing/feeding your baby. This will be given home with you when your baby is discharged for you to refer back to if needed.